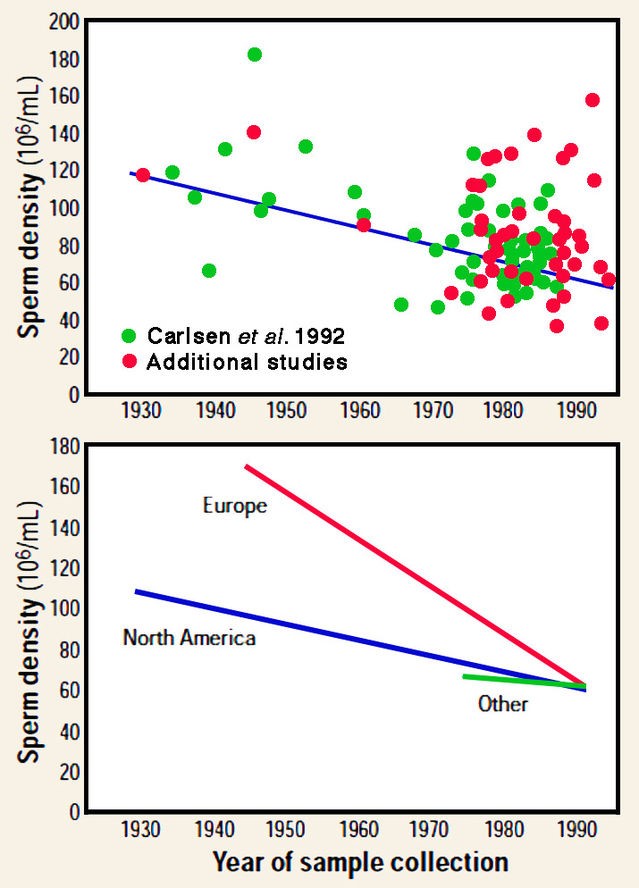
It's difficult to give figures for male infertility in Africa for several reasons: In the collective unconscious, infertility was often attributed to women, as was the sex of the child. We therefore need to set up national registers that can collate data from each country, taking into account polygamy, which can sometimes muddy the waters. That said, as on every continent, male fertility is declining as a result of environmental factors, pesticides and other endocrine disruptors that have a direct effect on the spermogram. Obesity, tobacco and other recreational drugs also have a detrimental effect on spermatogenesis. It is estimated that since the 1950s, sperm concentration has fallen by around half.
Infertile is more of a colloquial term, usually referred to as infertility. Infertility is defined as the absence of pregnancy after more than a year of unprotected intercourse between a couple. Of course, it's important to make sure that intercourse takes place during the ovulatory period, without any erectile or ejaculatory dysfunction.
Infertility puts you on the margins of society, and in North Africa, at least, it's mainly women who struggle to achieve pregnancy and assume a part of their femininity through motherhood. So it's usually with a visit to the gynaecologist that it all begins. Andrology is a new specialty, and any infertile man should also undergo a clinical examination by the andrologist, as well as a battery of tests, the first of which is the spermogram.
PMA is now a reality, and a large number of families have been formed through PMA, and unlike adoption, this is done without the knowledge of the entire family, which avoids stigmatizing each member of the couple.
Intrauterine insemination (IUI), IVF, ICSI, conventional testicular biopsy or microTESE, as well as anything involving the freezing and preservation of gametes or embryos.
MAP is indicated in cases of male, female or mixed infertility, or infertility of undetermined etiology, whenever natural procreation fails, or at the couple's request, particularly when stimulation is poorly tolerated by the partner. It is also indicated in cases of low ovarian reserve, or in couples where the partner is over 38.
Micro TESE dates back over 20 years and was first described using a microscope. Unfortunately, this technique is very time-consuming, so I use high-magnification magnifiers (x6), which enable me to obtain almost equivalent results for much less operating time. In a patient with non-obstructive azoospermia, conventional testicular biopsy is positive in 30 to 43% of cases, whereas the use of magnifying glasses gives a positivity rate of 52%. Similarly, in a man who has had a negative conventional BT, magnification enables us to catch up with around 1/3 of men who have been denied paternity. Magnification helps identify dilated seminiferous tubules, which are more likely to contain foci of residual spermatogenesis.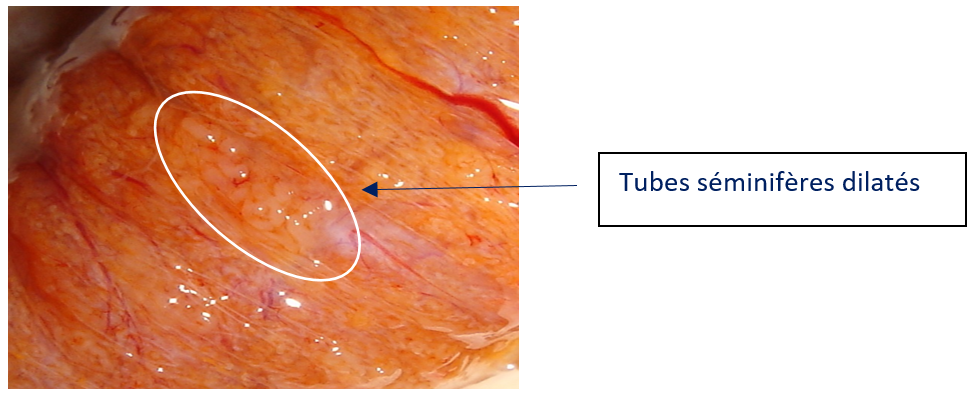
Intrauterine insemination is successful in around 15% of cases per cycle. IVF and ICSI have a pregnancy rate of 35-50% per cycle, and up to 60-70% in cumulative rates when frozen embryos are transferred.
The type of infertility, the age and ovarian reserve of the partner, and the quality of the sperm. The experience of the medical team naturally plays a decisive role!
MAP often creates stress within the couple, and this misunderstanding can sometimes drive the 2 partners apart, not forgetting that it can also be the cause of erectile dysfunction. It's also important not to involve the whole family in the couple's intimate affairs.
For many Africans, it's important to have a family, and a large one if possible! But this must be done within the precise framework of laws governing the transport, use and freezing of gametes. The andrologist has an important role to play, not only in the practice of mTESE, but also in identifying curable causes of infertility, which can sometimes avoid recourse to MAP.
It's a great initiative that keeps everyone informed and shares knowledge. Let's not forget that, to establish the new spermogram standards, the WHO called on American, European and Asian patients. So it's up to us to create our own networks and, why not, our own guidelines!


